Dr. Terencia, Dr, Bini Faizal(ENT), Dr, Bhanu Vikraraman Pillai Paed gastro), Dr. C Jayakumar
AIMS, KOCHI
A 5year old female child presented to ER with alleged historyof foreign body ingestion 2 days back following which she had complaints of throat pain, dysphagia and odynophagia.No h/o breathlessness or hematemesis. Foreignbody retrieval attempted in a local hospital near failed to retrieve. Xray chest and neck showed foreignbody in Cricopharynx. At AIMS examination showed normal Oral cavity and Oropharynx ,No palpable swelling/nodes in the neck,nose-Septum central and Ears and Bilateralintact tympanic membrane. Systemic examination was within normal limits.
Labs TC-14.2ku/ml, N-90%, L-5%,CRP-30mg/L, ESR-17mm/1st hr


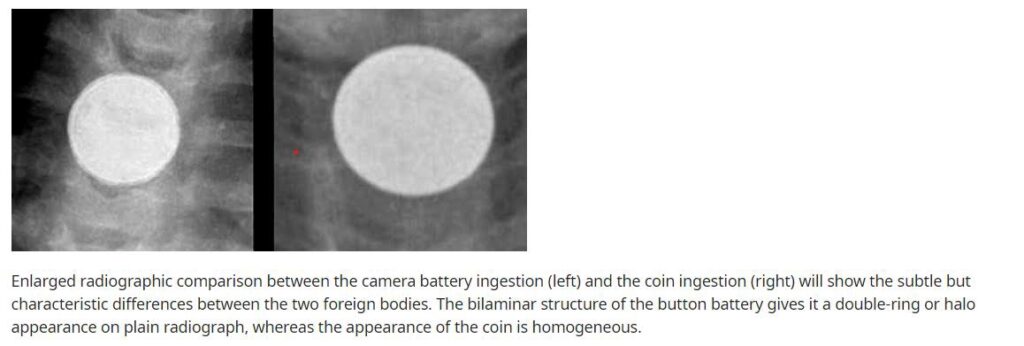
Fig-1 and 2 showing Xray STNL and CXR – Foreign bodyseen at the level of cricopharynx-probably Button
She underwent Esophagoscopy- with Foreign Body Removal (Emergency) under GA on 30/7/23. Under GA Scope was detected with difficulty in the cricopharyngeal area. Ulcerated areas on either side with necrotic material were seen. Battery was partially dislodged but could not be removed. Hence, direct esophagoscopy was used and endoscope was passed through esophagoscopy and foreign body was removed.
Figure 3- Direct esophagoscopy-Foreign body removal
Perioperative period was uneventful. Child was kept on RT feeds initially .She was given IVantibiotics for 7 days course. CT chest was taken on second postoperative day which showed NG tube in situ with no extraluminal pockets of air in mediastinum and with no significant abnormality along the course of the esophagus. On fourth postoperative day clear floods followed solid feeds orally on fifth postoperative day. Child was tolerating orally,had no complaints of aspiration.Child is being discharged with RT insitu.Child is being advised to continue RT +oral feeds for the next 3 weeks and was discharged with stable vitals.
Button battery ingestion children requires rapid recognition. Lithium batteries that are ≥20 mm in diameter are associated with esophageal impaction in children and can cause serious complications.
Most button battery ingestions are witnessed, and most children are asymptomatic at the time of presentation. The clinician should also maintain a high level of suspicion for an esophageal button battery, despite a negative history of ingestion, in young children with abrupt onset of any one of the following: Refusal of oral intake, Difficulty swallowing, Chest pain, Drooling, Hematemesis. Demonstration of the button battery on plain radiographs confirms ingestion.
For asymptomatic children with acute button battery ingestions (eg, witnessed or likely to have occurred within 12 hours) who are >1 year old and without allergies to honey or its components, we suggest one oral dose of pure honey (eg, 5 to 10 mL) be given at home the caregiver as soon as possible after ingestion.
Once in the emergency department, the child may receive another dose of honey or, if no history of allergy, a single dose of sucralfate 500 mg prior to radiography.Children with a delayed recognition of a button battery ingestion (eg, uncertain timing of ingestion, ≥12 hours after ingestion, or symptoms of serious esophageal or vascular injury or mediastinitis such as hematemesis, chest pain, or fever) should not receive honey or sucralfate and have no oral intake until the evaluation is complete.
We recommend emergency evaluation and plain radiography for patients who meet any one of the following criteria:
-All children under 12 years of age who ingest button batteries
-All patients who have ingested a button battery that is ≥12 mm in diameter
-All patients for whom the diameter of the button battery is not known
Management – Management of ingested button batteries depends on its location, symptoms, and size:
Esophageal impaction – For patients with button batteries that are lodged in the esophagus, we recommend emergency removal with direct endoscopic visualization an appropriate specialist
Gastric location – For patients who have a button battery in the stomach and who have signs or symptoms of esophagealor gastric injury at initial presentation, even if minor, we suggest emergency endoscopy and removal
Intestinal location – Button batteries that have cleared the stomach typically exit the gastrointestinal tract within one week. Patients with symptoms of abdominal pain, hematochezia, or fever without confirmed battery passage warrant urgent evaluation, emergency radiography, and, if radiographs demonstrate a retained intestinal button battery, prompt surgical consultation for removal.
Follow-up radiographs should be performed in asymptomatic patients with an intestinal button battery who have not passed the battery 10 to 14 days, regardless of size. (See ‘Intestinal location’ above.)
Asymptomatic ingestion of small button battery – Asymptomatic, healthy patients >12 years of age with confirmed ingestion of a solitary button battery that is ≤12 mm in diameter and without co-ingestion of a magnet may undergo observation for battery passage at home without initial radiographs as long as the patient or caregiver is reliable and able to promptly seek treatment should symptoms develop. Radiographic localization is warranted if battery passage is not confirmed in 10 to 14 days.
TAKEAWAY MESSAGE- Its essential to anticipate esophageal button battery, despite a negative history of ingestion when an infant or toddler presents with abrupt onset of refusal of oral intake, Difficulty in swallowing, Drooling orHematemesis and to proceed with further radiological evaluation and management for foreign body location and removal.
