Dr.Venkat Kumar Raju , Dr. Bhanu Vikraman Pillai, Dr C Jayakumar
Five yr old girl is a known case of ileal Atresia Type 2, S/p Bishop Koop anastomosis on day 3 of life, Biliary atresia, S/p Kasai portoenterostomy at 3 month, Chronic liver disease
She presented with 3episodes of fresh bleeding per rectum of moderate quantity since two days .She also had brief episode of loss of consciousness before reaching here.
On Admission
Child was drowsy
Pale +, Icteric +, Clubbing +
No lymphadenopathy and edema
On systemic examination
RS- bilateral scattered ronchi
GIT-right subcoastal healed scar, liver 3cm firm in consistency , with sharp borders, spleen of 4cm
No Ascitis
CNS- GCS 13 no deficit
Due to Acute GI bleed she was shifted to PICU
VBG done showed severe metabolic acidosis,
Initial labs showed severe microcytic hypo chronic anemia with thrombocytopenia and negative inflammatory markers

She continued to have bleeding per rectum She was started on IV Ocreotide.
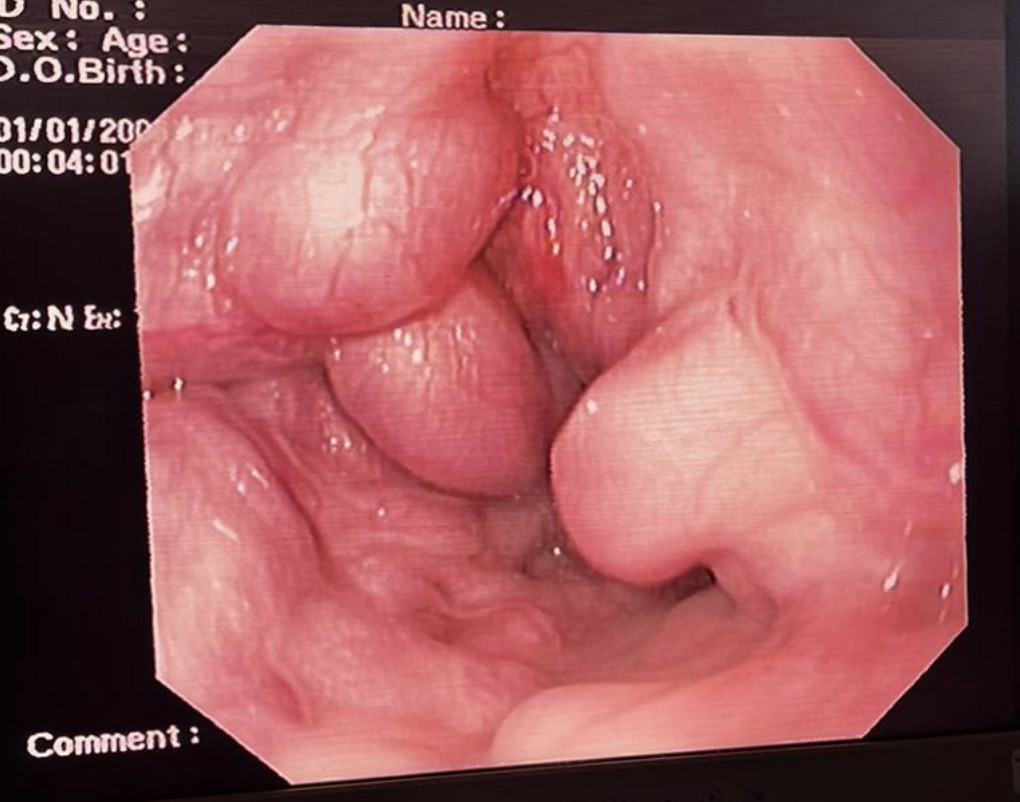
Emergency OGD scopy was done , found to have oesophageal varies and ligation was done endoscopically under general Anasthesia.
Sigmoidoscopy was avoided due to poor preparation of bowel
Her saturation dropped to 70% when she was tried to wean off oxygen . In view of oxygen dependency and clubbing , Hepatopulmonary syndrome was considered.
Contrast Enhanced ECHO was done which showed pulmonary A-V Malformations, which was suggestive of hepatopulmonary syndrome
A liver transplant consultation was taken ,Lung perfusion scintigraphy was done to asses the severity , she was found to have significant systemic shunt
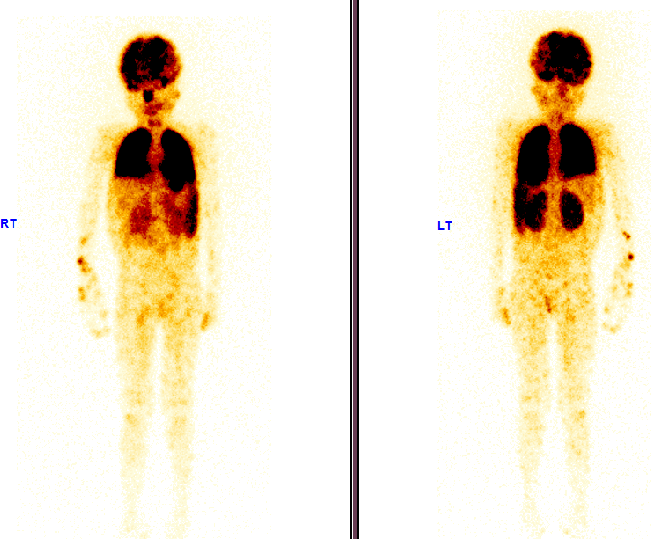
The above image is Lung perfusion scan , showing significant shunting from lungs to liver,brain and kidneys
Child was discharged on home o2, parents were explained about her condition
Her mother was worked up as her donor
After 3 months
She was admitted for transplant , post transplant she had a very severe portal vein thrombosis , and succumbed to her illness.
Discussion-
Hepatopulmonary syndrome (HPS) is a complication that can result from liver cirrhosis or portal hypertension. This causes progressive symptoms such as dyspnea and cyanosis. The precise mechanism of HPS development is not fully understood. Increased bacterial translocation and endotoxin in cirrhosis leads to overproduction of vasodilatory substances such as nitric oxide (NO )
Increased NO and pulmonary angiogenesis result in dilated pulmonary capillaries and ventilation–perfusion mismatch.
HPS has three distinct features: liver disease, hypoxemia, and intrapulmonary vasodilation.Alveolar-arterial oxygen gradient (PA-aO2) measurements are accurate measurements of hypoxemia. However, arterial blood gas analysis (ABGA) is impractical for pediatrics and is accompanied complications such as arterial spasm and hematoma.
For screening patients with HPS with cirrhosis, pulse oximetry has been validated as a screening tool.
The threshold of a pulse oximeter ≤ 97% has been shown to detect PaO2 levels below 70 mm Hg with 100% sensitivity and 65% specificity. Two methods can be used to identify intrapulmonary vasodilation: contrast enhanced echocardiography (CEE), most often using microbubbles as the contrast, and radioactive lung perfusion scan using macroaggregated albumin (MAA).
An effective medical therapy for HPS has yet to be established. Liver transplantation (LT) remains the only effective treatment for HPS. The occurrence of HPS is associated with increased morbidity and mortality
In particular, HPS is a progressive disease and the outcome is poor if the degree is severe before LT.Uncommon Complication of Chronic liver disease
Take home message
The takeaway is to be vigilant for hepatopulmonary syndrome in children with chronic liver disease, as it can lead to significant increase in mortality . Early recognition and management are crucial for improving outcomes and to do an early transplant
