Dr. Adeena D S
Dr Sajith Kesavan(Paed pulmonologist and intensive st,Dr Greeshma Issac(intensivist)Dr Praveena,
Dr C Jayakumar
AIMS,kochi
Eleven year old boy presented with complaints of left hip pain of 1 week duration after trauma during sports at school and inability to bear weight since 2 days.H/o an abrasion wound over left elbow few days prior to onset of pain.He was on IV antibiotics,but soon developed breathing difficulty with chest xray findings of bilateral diffuse haziness.In view of worsening of distress and altered sensorium, child was referred to AIMS
Other history is normal
At admission, tachypneic and sick- looking with altered sensorium.
Maintaining saturation on 6 litres of oxygen via face mask , BP-80/52mmHg,HR-130/min
Fluid filled lesions over face,ulcer over left elbow, Non blanchable erythema over bilateral hips.
Chest- tachypnoeic, SCR+, AEBE, b/l scattered creps+
CVS:Heart sounds muffled
P/A soft not distended
CNS- drowsy , altered sensorium.
Labs CRP value(382), procal(>100), with leucopenia, transaminitis, thrombocytopenia with elevated ferritin (4079) and LDH (728) levels.
Dengue, lepto, salmonella were negative. Chest Xray showed bilateral pulmonary infiltrates suggestive of ARDS.
He was started on BIPAP initially.
Bedside ECHO showed evidence of myocarditis with severe LV dysfunction and severe refractory shock.
He was intubated, mechanically ventilated and bifemoral VA-ECMO intiated.
He required multiple vasoactive agents, steroids.
Skin lesions were suggestive of Staphylococcal scalded skin syndrome,and considering systemic involvement a provisional diagnosis of Toxic shock syndrome was made.
He also received IVIG. Wound debridement was done and tissue and swab were sent for C/S. Blood culture sent was positive for Methicillin sensitive staph Aureus. BAL and wound cultures also grew Staph Aureus. He was initially started on ceftriaxone and was upgraded to Piptaz, Teicoplanin, Clindamycin and Flucloxacillin.
After 72 hours on ECMO he improved and clearing of lung fields was seen on CXR. After an ECMO clamp off trial ,which he tolerated well , he was de-cannulated the next day but continued on mechanical ventilator support and on multiple inotropes infusions,that were later tapered and stopped. Later BAL culture grew ESBL Klebsiella and Candida tropicalis, hence antibiotics were changed to Ertapenem, Clindamycin was changed to Linezolid. In view of the pain over anterior aspect of thigh and inability to bear weight, left hip septic arthritis was considered. He had persistent fever spikes,whole body MRI done,showed signal intensity in left superior pubic ramus and ischium – suspicious of osteomyelitis. Multiple small ill defined, mostly deep seated,collections were noted in left hemipelvis and upper thigh.
Mild hip joint effusion, with synovial enhancement was present.
He underwent Arthrotomy and washout of left hip that showed edmatous fluid in myofascial planes. Synovial fluid aspirate from the joint cavity was sent for HPE and
C/S. Bone sample taken for biopsy showed fibrocollagenous tissue with areas of necrosis and mixed inflammatory infiltrates .In view of clinical worsening and septic arthritis, antibiotics were upgraded to ceftazideme-avibactem-aztreonam with vancomycin, flucloxacillin, colisitin and micafungin.
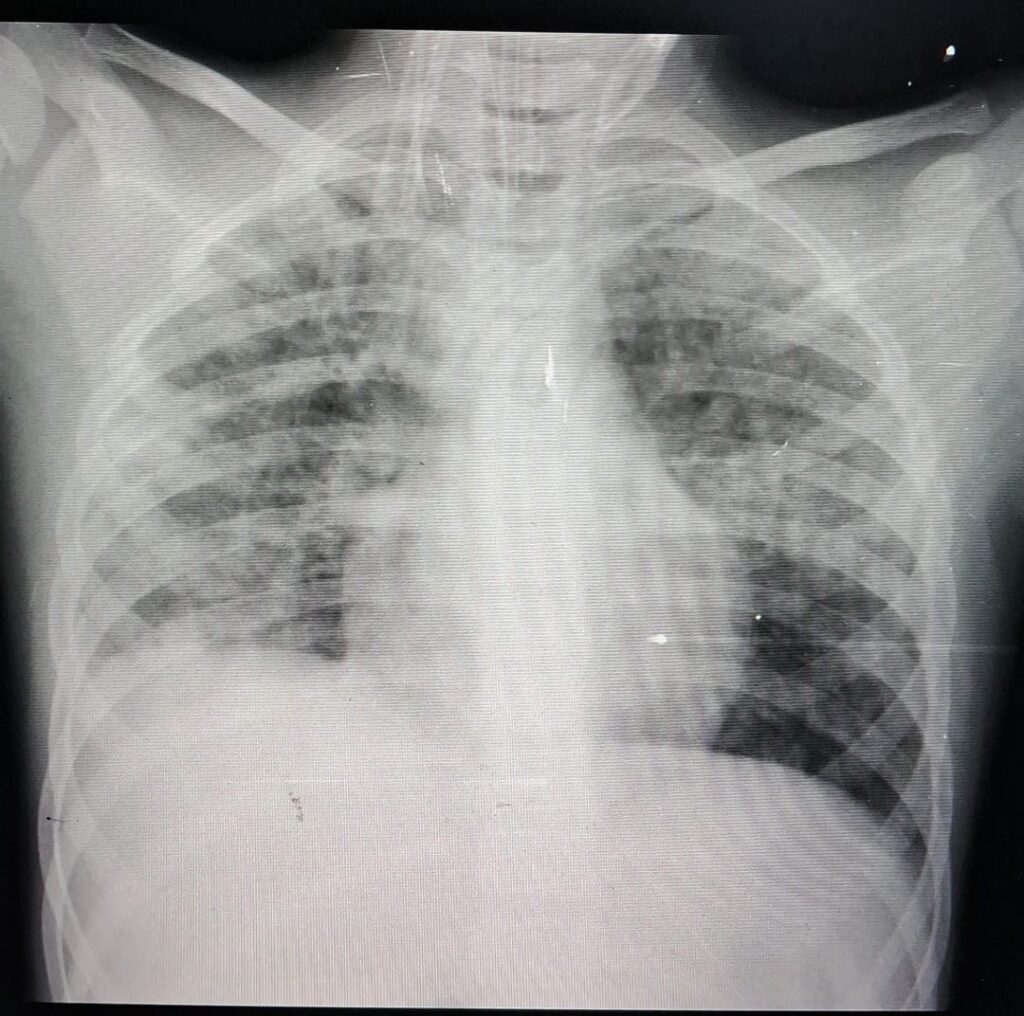
Following decannulation of ECMO,he was started on appropriate anticoagulation regimen for DVT propylaxis, and physiotherapy. During the hospital stay, he had developed AKI, dyselectrolemia and ischemic hepatitis, all of which were managed and he improved well. His serial X rays and ABGs showed improvement with resolution of ARDS and was he was extubated to BIPAP and subsequntly weaned off to room air and shifted to ward.
Repeat USG Lt Hip done showed an irregular collection,deep subcutaneous plane along the upper lateral aspect of left thigh measuring 4.7 x 1.4cm. Repeat MRI done showed features of osteomyelitis involving left superior pubic ramus, ischium & left hip joint efusion with extensive soft tissue and muscle edema involving left hemipelvis and upper thigh. PET MRI Scan showed features suggestive of acute osteomyelitis and enlarged lymphnodes suggestive of infective or inflammatory changes.
A repeat left hip arthrotomy and washout was done and samples were sent for cultures and gram smear. Cultures were sterile, BIOFIRE detected MSSA.Cefipime and Gentamicin were added on and Flucloxacillin was continued and later changed to oral Dicloxacillin and planned to continue for 6 weeks.
Echo was done to rule out endocarditis.USG Abdomen showed hepatosplenomegaly.Rigorous nutritional and physical rehabilitation was done given during the course of hospital stay. Repeat Blood investigations and chest Xrays done showed improving trends. Left elbow wound was healing well with no sinus tracts or discharge.He was discharged on onal dicloxacillin with advice to be under close follow
Toxic shock syndrome -(TSS)
An acute illness with fever,hypotension,rash and end organ damage.most commonly caused a toxigenic strain of Staphylococcus aureus or group A streptococci.
Non- menstrual settings where TSS occur are soft tissue infection, burns, retained foreign bodies etc.
The condition is toxin mediated.
The superantigens pass the normal pathway for activation of T cells resulting in over-activation of cytokines and inflammatory cells.
Treatment include aggressive management of shock,broad spectrum antibiotics- vancomycin or linezolid.
Clindamycin to supress toxin production. IVIG is thought to work neutralizing the activity of toxins.The case fatality rate of streptococcal TSS is as high as 50%.
