Dr Varsha V S, Dr Suhas Udayakumaran, (Paediatric neuro surgeon )Dr Praveena N Bhaskaran, Dr Navya George DrCJayakumar
Department of Pediatrics AIMS Kochi.
Fifteen year old boy presented with c/o headache and intermittent fever of 1 month duration. As he had persistent headache with sinus tenderness and low grade fever he was on oral antibiotics as per the advice of ENT surgeon
But symptoms got worsened with increasing severity of headache and appearance of tender swelling in the forehead. At this juncture he had parenteral antibiotics
But he developed 2 episodes of generalized tonic clonic seizures
MRI done at this time showed left frontal abscess.
After the imaging child came to AIMS
He was drowsy and febrile, with PR: 100/min, BP: 120/80mmhg, RR: 18/min, SpO2: 100% RA, and GCS of 12/15.
Neurological examination done showed normal tone.
DTR++ and no meningeal signs of irritation. Other system examination done were normal.
Local examination done over the forehead showed firm, tender swelling measuring 1x2cm.
Transillumination done was negative. Labs showed neutrophilic leucocytosis with highly elevated CRP (217mg/L).
RFT, LFT, SE were normal.
Ammonia and lactate were normal.
Preop serology and Immunoglobulin profile were normal. He was started with IV broad spectrum antibiotics and supportives.
Diagnosis
Clinical possibility of Pott’s puffy tumor or sub dural abscess were considered.
CT Brain and paranasal sinuses were taken which showed small left frontal abscess with neuro-parenchymal edema.
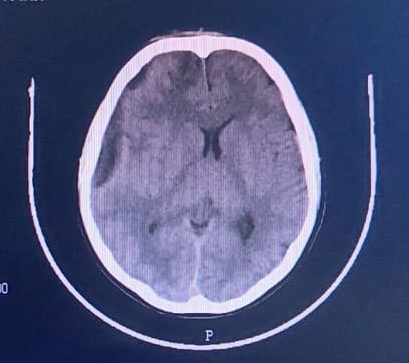
Pic 1 : CT Brain showing small left frontal abscess with neuro-parenchymal edema.
He underwent aspiration of abscess which showed purulent foul smelling pus and send for c/s. Pus c/s showed streptococcus and pseudomonas and antibiotics were changed as per culture sensitivity. Subsequently diagnostic trans nasal endoscopy (DNE)was done and showed B/l congested nasal cavities, high DNS to right side, discharge noted in medial and lateral part of middle turbinate on both nasal cavities probably in frontal recess
He was gradually improving for 3 days, after which he had severe headache and CT brain was repeated which showed increase in size of the right fronto-temporal subdural collection with worsening midline shift. So diagnosis of right fronto temporo parietal subdural empyema with right bifrontal cerebritis secondary to frontal sinusitis was made.
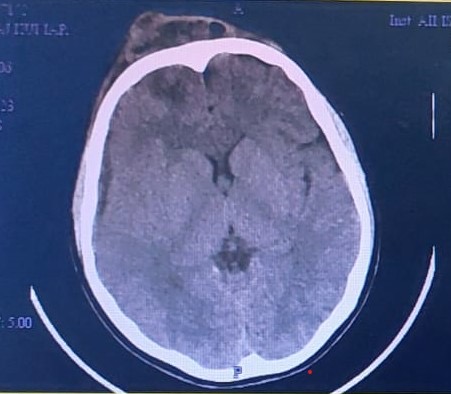
Pic 2: CT Brain showing right fronto temporo parietal subdural empyema.
He underwent right tempero parietal burr hole and evacuation of subdural collection. Antibiotics were continued according to the culture sensititvity reports.
Repeat DNE was done which showed significant improvement and resolving sinusitis.
He improved symptomatically and had no further seizures. He completed 21 days of IV antibiotics. He was advised to continue levetiracetam
Intracranial subdural empyema also known as subdural abscess/cortical abscess/purulent pachymeningitis/ phlegmonic meningitis/ subdural suppuration, is a loculated collection of pus in the subdural space between the dura mater and the arachnoid.
The etiology of subdural empyema include prior cranial surgery, head trauma with open skull fractures, or penetrating injury, infected hematoma or subdural effusion, and not properly treated ear and sinus infections.
Forty to 80% of patients with subdural empyema have otorhinologic infections, especially paranasal sinuses.
Common microorganisms are
Anaerobes,
Aerobic Streptococci,
Staphylococci,
Haemophilus influenzae,
Streptococcus pneumoniae
Gram-negative bacilli.
In cases of subdural empyema secondary to paranasal sinusitis, the most common microorganisms reported have been anaerobic and microaerophilic streptococci (Streptococcus milleri and Streptococcus anginosus).
Following cranial trauma or surgical procedures, the most common organism is Staphylococcus aureus. Coagulase-negative Staphylococci, anaerobes, Gram-negative organisms can also be found in those cases of trauma or surgical procedures.
Subdural empyema most often occurs due to the direct extension of local infection. The infection can spread to the intracranial compartment due to the valveless diploic veins of Breschet.
A subdural empyema must be considered in a patient diagnosed with sinusitis or otitis who develops a fever, headache, and cranial pain.
History and physical examination should help tailor case evaluation and diagnosis; however, cranial imaging should be performed in all patients with suspected subdural empyema.
Subdural empyema appears as a hypodense area over the cerebral hemisphere or along the falx better with a contrast computed tomography scan.
The diagnostic imaging study of choice for intracranial subdural empyema is magnetic resonance imaging (MRI) with intravenous gadolinium enhancement.
Imaging findings are usually described as a crescent-shaped or elliptical area of hypointensity on T1-weighted images underneath the skull
Spinal puncture is not indicated for the diagnosis and can be dangerous in those patients with increased intracranial pressure and empyemas, causing mass effects.
The treatment of cranial subdural empyema is multimodal, including both medical and surgical treatment.
Treatment options including multiple burr holes or a craniotomy for drainage and debridement with antibiotic coverage. A craniotomy usually offers better results and fewer recurrences.
Awake and alert patients have a good prognosis in the majority of the cases. Stuporous and comatose patients have high mortality.
Up to half of the patients have permanent residual neurological deficits. Late seizures may occur despite the use of antiepileptic medications. An unfavorable prognosis can be seen in cases of brain herniation.
Complications of subdural empyema include seizures, cerebritis, cerebral abscess, cerebral edema, cortical venous thrombosis with cerebral venous infarction, cavernous sinus thrombosis, sepsis, septic shock, electrolyte imbalances, hydrocephalus, cranial osteomyelitis in adjacent cranial bones, osteomyelitis of the craniotomy bone flap, and residual neurological deficits.
The key take home message
Sinusitis is not simple
Full 10 days courses of antibiotics is needed after symptom resolution in case of sinusitis
