Dr Varsha V S,Dr Anil Mathew(Paed Nephrologist)(Dr Sajith Kesavan,Dr Greeshma Issac;Pead intensivists)DrC Jayakumar
Department of Pediatrics , AIMS Kochi.
Two years old boy presented to ER with c/o fever and generalised edema of 2 days duration. He was evaluated outside with urine and urine protein was >3+ and urine protein creatinine ratio> 0.2 ,with hypoalbuminemia . Persistent edema was the reason for referral
Vitals: Afebrile, PR: 70/min, BP: 90/70 (within 50th centile), RR: 28/min, SpO2: 98%RA.
Systemic examination done was normal.
Labs done initially showed neutrophilc leucocytosis with negative inflammatory markers.
Hypoalbuminemia with urinary proteinuria, hyper cholestrolemia and hyper triglyceridemia was present with normal RFT. Child was started on prednisolone 60mg/m2.
On day 3 of admission he developed high grade fever with poor oral intake, hypotension with worsening of sensorium (8/15) and was shifted immediately to PICU suspecting septic shock and required intubation and mechanical ventilation with fluid resuscitation and inotropes.
Labs done showed highly elevated CRP (335mg/L) and procalcitonin (100), highly elevated counts which is neutrophilic predominant.
Antibiotics were hiked to meropenam. CSF study done showed streptococcal pneumonia encephalitis.
MRI brain done showed multiple near symmetrical linear areas of diffusion restriction radiating from ventricle seen in white matter of bilateral neuroparenchyma, predominantly frontal lobes- could represent encephalitis.

Fig 1: MRI image showing features of encephalitis.
Antibiotics were changed to IV ceftriaxone and vancomycin. He was off ionotropic support on day 2 of PICU admission. His sensorium improved and was extubated on day 4. Repeat MRI done showed multiple linear areas of T2 FLAIR hyperintensity showing diffusion restriction in the periventricular white matter of bilateral frontal lobes. These more conspicuous when compared to the prior study. No new areas of diffusion restriction. No enhancing lesions. He was planned to continue antibiotics for 21 days. He was clinically improving.
On day 6 of PICU stay he was noticed to have paucity of limb movements on left side. Urgent MRI brain was done showed acute infarct involving genu and posterior limb of right internal capsule. Focal thrombus involving mid part of the superior sagittal sinus and suspicious thrombus in the left cortical veins. Bilateral subdural collections causing mild mass effect on the adjacent cerebral parenchyma and right frontal lobes – Suggestive of hygroma. MRA/ MRV showed thrombus in the left cortical vein. Other major vessels are patent. T1/T2 hyperintensities in the left frontal subdural region showing blooming and diffusion restriction suggestive of blood products in the anterior subdural space.
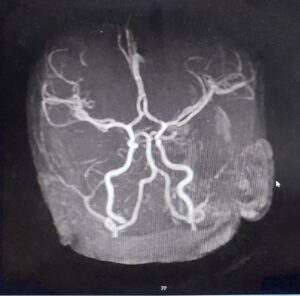
Fig 2 : MRA/MRV showing cortical venous thrombosis.
He was diagnosed to have Complicated Nephrotic Syndrome (Streptococcal encephalitis and cortical vein thrombosis).Stroke medicine consultation was sought and hence started on antiplatelet (aspirin). Neurosurgery opinion was sought in view of the MRI findings and he was advised observation.
On observation there was no worsening of symptoms and he was shifted to ward. He was given supportive management with physiotherapy. He improved gradually and was discharged with stable vitals and other lab parameters. Planned to keep under close follow up.
Nephrotic syndrome is defined the presence of heavy proteinuria (>1 g/m2; spot urine protein/ creatinine >2 mg/mg), hypoalbuminemia (albumin3.0 g/dL), and edema. The usual age at onset is between 1 and 12 years. Most cases in childhood are idiopathic, and an underlying systemic illness is seen in<10% of patients. More than 80–85% of children with nephrotic syndrome show remission of Proteinuria following therapy with corticosteroid and have good outcome.
Differential diagnosis: Protein losing enteropathy, hepatic failure, heart failure, acute or chronic glomerulonephritis, and protein malnutrition, insect bite.
Investigations: Baseline:
1. Urinalysis and urine microscopy
2. Urine albumin or protein:creatinine ratio
3. 24-hr timed collection of urine for protein quantification
4. Serum electrolytes, albumin, total protein, renal function, and cholesterol
If suspecting glomerulonephritis:
1. Serum complement C3 and C4 concentrations
2. Serum immunoglobulins
3. Antistreptolysin titers
4. Anti-DNase B antibodies
5. Antinuclear antigen antibodies
6. Anti–double-stranded DNA antibodies
7. Anti-neutrophil cytoplasmic antibodies
Renal Biopsy indicated in
1. Persistent or sustained elevation in creatinine
2. Age<1 years/>12 yrs.
3. Significant hematuria or gross hematuria
4. Hypocomplementemia
5. Findings indicative of another autoimmune disease
6. Infection with hepatitis B or C, HIV, or tuberculosis
7. Hypertension.
Complications
Complications include frequent relapses, steroid resistance, hypovolemia and even acute kidney injury. Serious infections, including bacteremia and peritonitis (particularly Streptococcus pneumoniae, Escherichia coli, or Klebsiella), may occur due to urinary loss of immunoglobulins and complement. Throm-boembolism (TE) including deep vein thrombosis, central sinus thrombosis, renal vein thrombosis, and pulmonary embolism may occur due to a hypercoagulable state caused urinary losses of coagulation factors, antithrombin, and plasminogen.
Prognosis: Depends on steroid responsiveness. Steroid resistant nephrotic syndrome have higher propensity to progress to End stage kidney disease when compared to steroid dependent.
