Dr. Venkat Kumar Raju, Dr.Krishna Kumar ,Dr.C Jayakumar
Ten year-old male presented with progressive abdominal distention of 3 months duration and breathlessness on exertion of 1 month duration. There was no history of fever, yellowish discoloration of skin and eyes, No bleeding manifestations.a His urine out put was normal and not frothy
On Examination, he had stable vitals, No pallor, icterus, cyanosis, clubbing, edema, and lymphadenopathy.Firmish non tender liver of 5cm below the rt costal margin was noted had Shifting dullness
CVS examination showed Elevated JVP Apex felt at 5th space outside the mid claviclular line. S1, S2 normal with no murmur ,no muffling with normal split in the pulmonary area.
At this Point our D/D were
- Cardio myopathy
- Constrictive pericarditis
- Budd Chiari syndrome
- Rheumatic disease
- Malignancy
Blood routines , LFTs were within normal limits
USG abdomens showed hepatomegaly with dilated veins and IVC along with moderate ascites and left sided pleural effusion
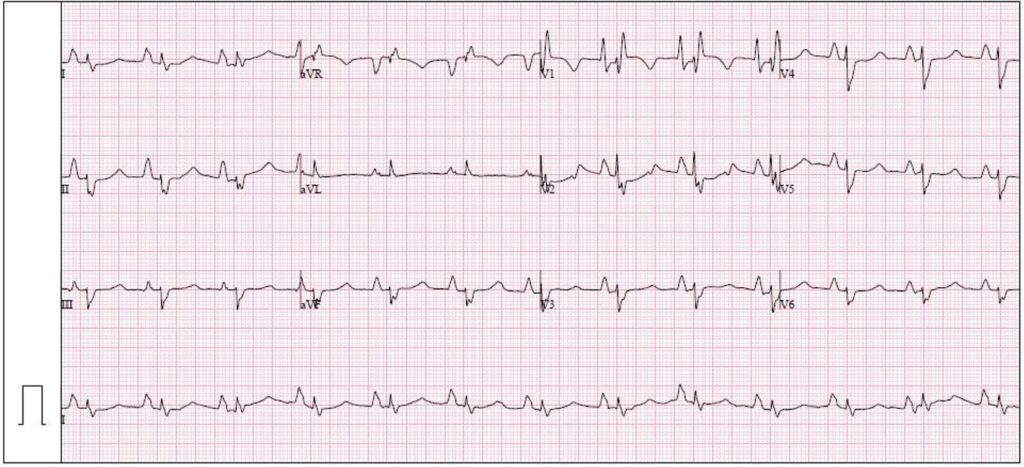
ECG done
P wave- Bi-atrial enlargement
Low voltage QRS
Right bundle branch block
Left bundle branch block
Chest X ray don
Cardiomegaly, RA/RV enlarged, RV type apex, SVC dilated
ECHO Done
Showed Restrictive Cardiomyopathy, Biatrial enlargement with Grade 3 diastolic dysfunction. Moderate PAH
Diagnosis- Restrictive cardiomyopathy

Genetics Studies were planned on follow up
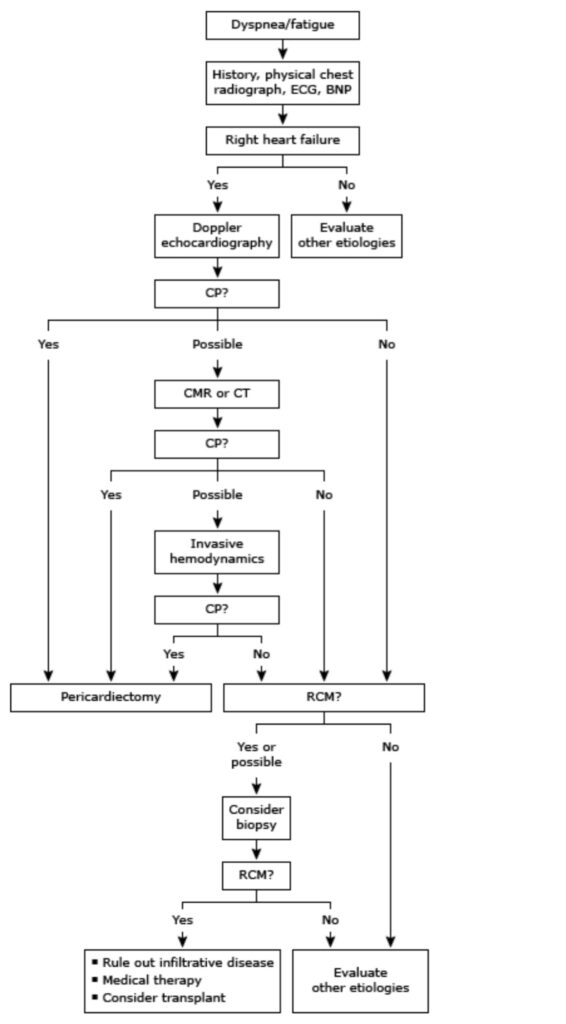
How to differentiate RCM vs Constrictive pericarditis
Etiology of RCM
Infiltrative disorders – RCM can be caused infiltration of the myocardium protein (eg, amyloid), iron, eosinophils, carbohydrate, fat, metabolic products (eg, cystine), and tumors. RCM can also be caused an inborn error of metabolism that results in myocardial infiltration carbohydrate (eg, mucopolysaccharide) or fat (eg, sphingolipid)
●Inflammatory disorders – Cardiac sarcoidosis can present as an RCM or as a dilated cardiomyopathy.
●Treatment-related cardiotoxicity – RCM is commonly caused a variety of medical treatments, with the most common being mediastinal radiation. Radiation therapy for breast cancer, Hodgkin lymphoma, and other chest malignancies may damage cardiac structures, causing fibrosis of the myocardium and resulting in an RCM, sometimes many years after initial treatment . The extent of radiation injury depends upon the strength of radiation and the response of the affected structures.
●Genetic causes – Gene variants represent an important cause of RCM, and variants in genes encoding myosin, troponin, titin, actin, lamin, desmoplakin, desmin, BAG cochaperone 3, and filamin C have all been associated with RCM phenotypes Many of the gene variants known to cause RCM overlap with gene variants that cause hypertrophic cardiomyopathy
●Other causes – Scleroderma, Noonan syndrome, and Werner syndrome are rare or uncertain causes of RCM
●Idiopathic – RCM is considered idiopathic if no underlying etiology can be identified after a comprehensive diagnostic evaluation.
Treatment of the underlying cause — In patients who have an underlying cause of RCM, we treat the underlying cause as appropriate. Medications associated with RCM (eg, HCQ) should be discontinued. Treatment of certain underlying diseases associated with RCM (such as amyloidosis, sarcoidosis, and hemochromatosis) may increase survival, improve quality of life, and delay the need for heart transplantation. The management of these disorders is discussed in detail separately:
General management
Volume management — The general approach to volume management in patients with RCM is similar to that used for other forms of HF. Such an approach consists of the following components:
●The use of diuretics.
●The use of echocardiography and pulmonary artery catheterization to assess volume status.
●Referral of patients with moderate to severe HF to a chronic disease management program.
Heart failure therapies — Most of the pharmacologic and device therapies used to manage patients with other forms of HF (HF with reduced ejection fraction [HFrEF] or HF with preserved ejection fraction [HFpEF]) have not been shown to be beneficial or feasible in the management of patients with RCM. Our approach to the use of these therapies is based primarily upon
●We do not routinely administer agents that are commonly used to treat patients with HFrEF or HFpEF, such as renin-angiotensin-aldosterone system inhibitors, neprilysin inhibitors, beta blockers, and sodium-glucose cotransporter-2 (SGLT-2) inhibitors, since there is no evidence to support their use in patients with RCM. However, such therapies may be used for the treatment of specific indications (eg, angiotensin-converting enzyme inhibitors for treatment of hypertension, beta blockers for rate control of atrial fibrillation, or SGLT-2 inhibitors for treatment of diabetes).
●For patients with severely decompensated RCM, we do not routinely use of intravenous vasodilator therapy
(eg, nitroprusside, nitroglycerin, hydralazine) to treat refractory HF.
Management of arrhythmias — Patients with RCM who have atrial fibrillation should be treated similarly to patients with other forms of HF
End-organ dysfunction — In our experience, end-organ dysfunction is more common and less likely to be reversible in patients with RCM compared with other forms of HF. Thus, patients with RCM may require additional testing to detect and manage end-organ dysfunction. The diagnosis and treatment of syndromes commonly encountered in RCM include:
●Liver congestion and cirrhosis.
●Chronic kidney disease.
●Pulmonary hypertension.
Heart transplantation — Heart transplantation may be of benefit to patients with RCM who have treatment-refractory HF symptoms and are considered to have reasonable long-term survival. Similar to all patients with advanced HF, early referral (eg, before end-organ dysfunction is severe or irreversible) may increase the likelihood of successful transplantation. Indications and contraindications for heart transplantation
Take Home message – its crucial for pediatricians to explore cardiac origins when hepatomegaly appears without jaundice. A meticulous examination today safeguards a healthier tomorrow for our precious patients
