Dr. Venumadhav, Dr. C. Jayakumar
Department of Pediatrics, Amrita Institute of Medical Sciences
Introduction
A one year eleven month old male child presented with alleged ingestion of turpentine oil .
He was managed for the same at an outside hospital with high-grade fever, cough, and fast breathing of one week’s duration
As symptoms persisted, the child was referred here for further evaluation and management.
All other pediatric history and auxology was normal
There was no history of vomiting, chest retractions, confusion, decreased urine output, blood in urine, cyanosis, or seizures.
Examination and Investigations:
On examination, the child was febrile and tachypneic. Clinical examination showed decreased air entry on the right side. On percussion, a stony dull note was noted in the right axillary and infrascapular areas.
Based on the history of turpentine oil ingestion and clinical findings, a diagnosis of Chemical pneumonitiswith Pleural effusion or empyema was considerd. He was also monitored for other complications like hematuria, renal failure and hypotension.
Counts were elevated with markedly raised CRP ( TC-23k,N/L-61/27, CRP-288) . LFT,RFT, SE, done were within normal limits.
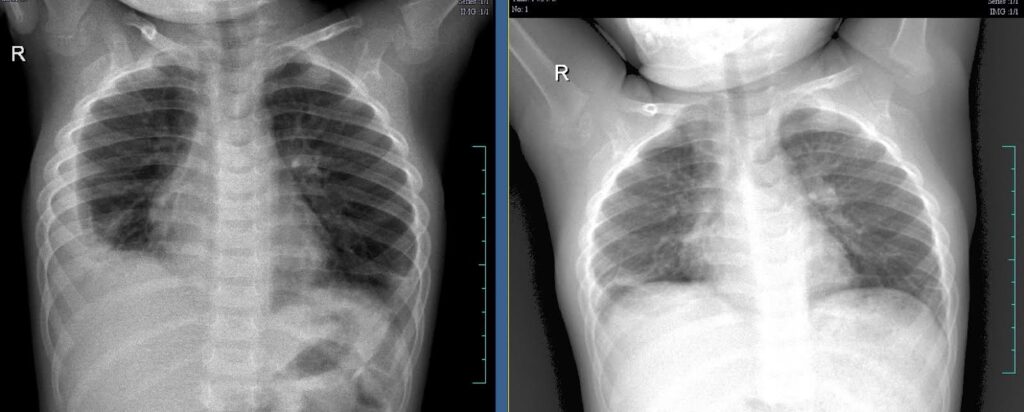
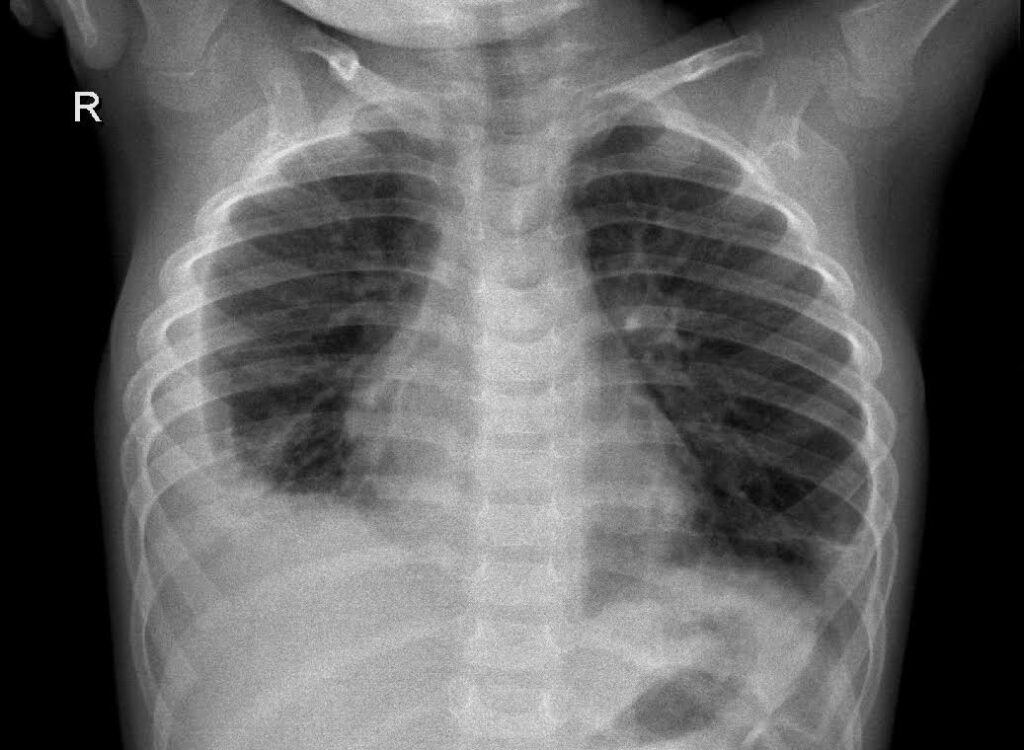
Chest Xray done showed obliteration of right costophrenic angle indicating likely of pleural effusion(Silhoutte sign positive)
USG Chest done showed organized thick walled echogenic right sided pleural collection is seen predominantly posterolaterally (Around 30cc) Multiple internal septations are seen with honeycombing appearance with trace pleural effusion and consolidatory changes of basal segments.
Pleural fluid tapping was done under aseptic condition.
Pleural fluid analysis was done (LDH-2241, TC-900) , which was suggestive of Exudative effusion.
Antibiotics were changed to Ampiclox and Amikacin (for providing borad spectrum coverage including staphylococcus). IV Antibiotics were given for 10 days ( A total of 21 days was planned, with d/s on Ampiclox for 11 more days). Repeat Counts , CRP , Xray showed marked improvement.
Comparing both Xrays before and after treatment
DISCUSSION:
Turpentine oil is a volatile essential oil derived from pine tree resin, mainly composed of alpha-pinene, beta-pinene, and other terpenes. It is commonly used in industrial applications such as solvent for paints, varnishes, and cleaning products. Historically, it was used topically for muscle pain, but medical use has declined due to its high toxicity. Turpentine oil is toxic if ingested, inhaled, or absorbed through the skin, especially dangerous in children.
Ingesting as little as 15 to 30 mL of turpentine oil can lead to serious poisoning in children. The toxicity primarily affects the gastrointestinal, respiratory, and central nervous systems. Symptoms of ingestion include nausea, vomiting, abdominal pain, and diarrhea. Respiratory issues like chemical pneumonitiscan occur due to aspiration, causing coughing, wheezing, and difficulty breathing. In severe cases, patients may develop pulmonary edema or respiratory failure.
Neurological symptoms include dizziness, headaches, and in severe cases, seizures or coma. Renal toxicitymay manifest as hematuria or oliguria. Cardiovascular effects such as hypotension or shock can occur in severe poisonings.
Chemical pneumonitis, a serious complication from turpentine aspiration, leads to inflammation of the lungs, causing chest pain, dyspnea, and fever. Untreated, it may progress to acute lung injury or ARDS (acute respiratory distress syndrome). Treatment focuses on airway management, oxygen therapy, and supportive care. Do not induce vomiting to prevent aspiration.
Activated charcoal is typically ineffective, and gastric lavage is rarely recommended unless done early with airway protection. Patients with respiratory distress may require mechanical ventilation. Corticosteroids are controversial for lung inflammation, and antibiotics are only used if infection is suspected. Complications include acute respiratory distress, central nervous system depression, and kidney failure. Early intervention is critical to prevent life-threatening outcomes.
