Dr.SreeLekshmys, Dr.C.Jayakumar, Dr.Praveena, Dr.Navya.
One yr old female child with history of one respiratory tract infection at six months of age, presented with high grade intermittent fever lower chest in drawing and fast breathing of 2days. At admission child was febrile and tachypneic with saturation of 93% improved to 99% with 5 L O. Decreased air entry noted at right mammary and infra axillary areas and b/L wheeze and scattered crackles . Labs Lymphocytic predominant CBC . Rapid antigen test was positive for Influenza A.
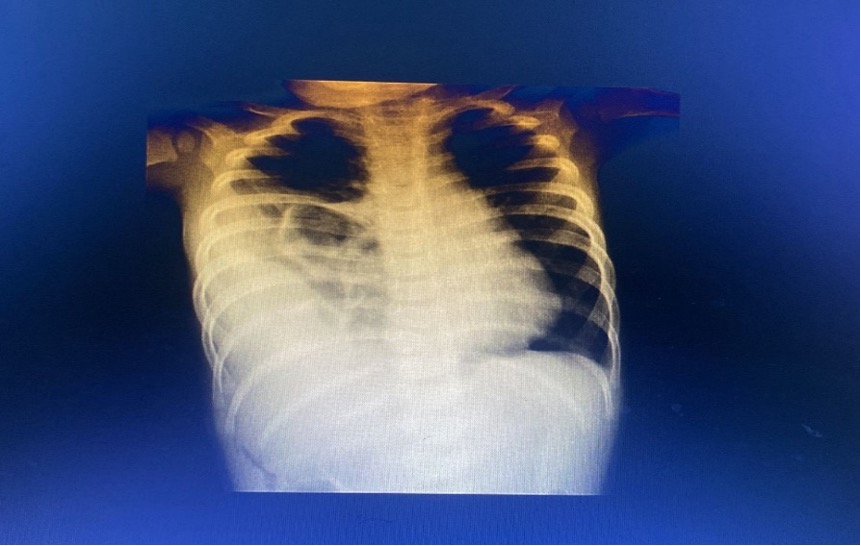
Chest xray revealed opacity involving right middle and lower zones.
Differentials
: Pneumonia with effusion,
Empyema,
Cystic lung lesion like CPAM
USG chest right upper quadrant and lower anterior chest fluid spaces with extensive dirty shadowing? effusion/ empyema/ bowel loops.

CECT chest showed large defect in the right hemidiaphragm with herniation of right lobe of liver, right kidney, right ureter, hepatic flexure of colon and small bowel loops with their vascular structures, causing collapse of right lower lobe, with an impression of right sided diaphragmatic hernia with herniation of abdominal viscera.
Diagnosis : Diaphragmatic hernia
Thoracoscopic CDH repair was planned once infection settles. She was managed with IV antibiotics (Ceftriaxone), Oseltamivir and nebulized bronchodilators. Child was gradually weaned of to room air day 4 of admission.
Discussion:
A diaphragmatic hernia is a communication between the abdominal and thoracic cavities with or without abdominal contents in the thorax.
The etiology is usually congenital and rarely traumatic . Defects can be in the posterolateral portion of the diaphragm (Bochdalek hernia ) – 90%, Retrosternal (foramen of Morgagni hernia) -2-6%.
The pathology of pulmonary hypoplasia and CDH includes abnormal septa in the terminal saccules, thickened alveoli, and thickened pulmonary arterioles. Biochemical abnormalities include relative surfactant deficiencies, increased glycogen in the alveoli, and decreased levels of phosphatidylcholine, total DNA,and total lung protein, all of which contribute to limited gas exchange.
Incidence is between 1 in 2,000 and 1 in 5,000 live births, females affected twice as often as males.
More common on the left (85%) , right(8-10%) and bilateral (<5%). Most cases are sporadic. Respiratory distress ( cardinal sign) immediately after birth or up to 48 hrs characterized tachypnea, grunting, use of accessory muscles, cyanosis, scaphoid abdomen, increased chest wall diameter, breath sounds may be heard in the chest, decreased breath sounds bilaterally.
Prenatal USG (b/w 16 & 24 weeks) shows polyhydramnios, chest mass, mediastinal shift, gastric bubble / liver in the thoracic cavity, fetal hydrops. Postnatally, Chest radiograph –confirms the diagnosis. In infants with an echogenic chest mass, further imaging is required. Differential diagnosis include Cystic lung lesion ( pulmonary sequestration, cystic adenomatoid malformation).
In the delivery room, infants with respiratory distress should be rapidly stabilized with endotracheal intubation. A preductal arterial oxygen saturation (SpO 2 ) value ≥85% should be the minimum goal. Conventional mechanical ventilation, high-frequency oscillatory ventilation (HFOV), and ECMO are the 3 main strategies to support respiratory failure in the newborn with CDH. Surgery is usually done 48 hr after stabilization and resolution of the pulmonary hypertension. Subcostal approach is most frequently used. Whenever possible, a primary repair using native tissue is performed. If the defect is too large, a porous polytetrafluoroethylene (Gore-Tex) patch is used. Higher recurrence rate in children with patches (the patch does not grow as the child grows) than in those with native tissue repairs. Following repair, the infant must be carefully monitored for worsening pulmonary hypertension. In some , a postoperative course of ECMO is needed
Carry home message
All cases of breathlessness are not due to pneumonia and andall the three modalities of investigation XRay ,USG and CT chest may be needed in some situations
