Dr.Venkatesh Kumar M, Dr.Suhas (Neurosurgery), Dr.C.Jayakumar, AIMS,Kochi.
Fourteen years old boy normal paediatric history presented with complaints of tilting (Oscillopsia)of of objects on prolonged observation since last one year.
He was in treatment for the same in the last one year with a diagnosis of vertigo and as hypoglycemic events . He had one epiosde of seizure in the past
No history of loss of consciousness further seizures, vomiting ,ENT bleed and head trauma after that incident
On examination, vitals stable. Head to foot examination did not reveal any neurocutaneous markers or facial dymorphism.
Auxology showed normal growth parameters. CNS examination unremarkable.CVS examination revealed short systolic murmur in the left upper sternal border. Other systems were within normal limits.
Differential considered at this point were:
1. Seizure disorder
2. Cerebral myeliod angiopathy.
3. Migraine and cluster headache
4. Beningn positional paroxysmal vertigo.
5. Moyamoya disease.
6. Intracranial space occupying lesions or congenital intracranial AV malformations.
Investigations:
Hemogram: TC- 15.08 K/uL, N/L: 74/17%, Hb-13, Plt-2.42 lkh.
Na+:137 mmol/l, K+:4.5 mmol/L, Ca2+: 9.43 mg/dl, Phosphorous: 4.1 mg/dl, Mg2+:2.2 mg/dl.
LFT,RFT, TFT: Normal
Ammonia:29.7 mmol/L, Lactate: 1.38 mmol/, CRP: 0.68 mg/L ,CPK: 245.
Vitamin-D:19.53 ng/ml , PT-INR: 13.5/0.96.
MRI Brain (done outside): 21x17x23 mm sized Arterio-venous malformation in Right Temporal region with feeders from M4 branch(branch of cortical part of middle cerebral artery ) of Right middle cerebral artery and draining into Superior sagittal sinus and Great cerebral vein.
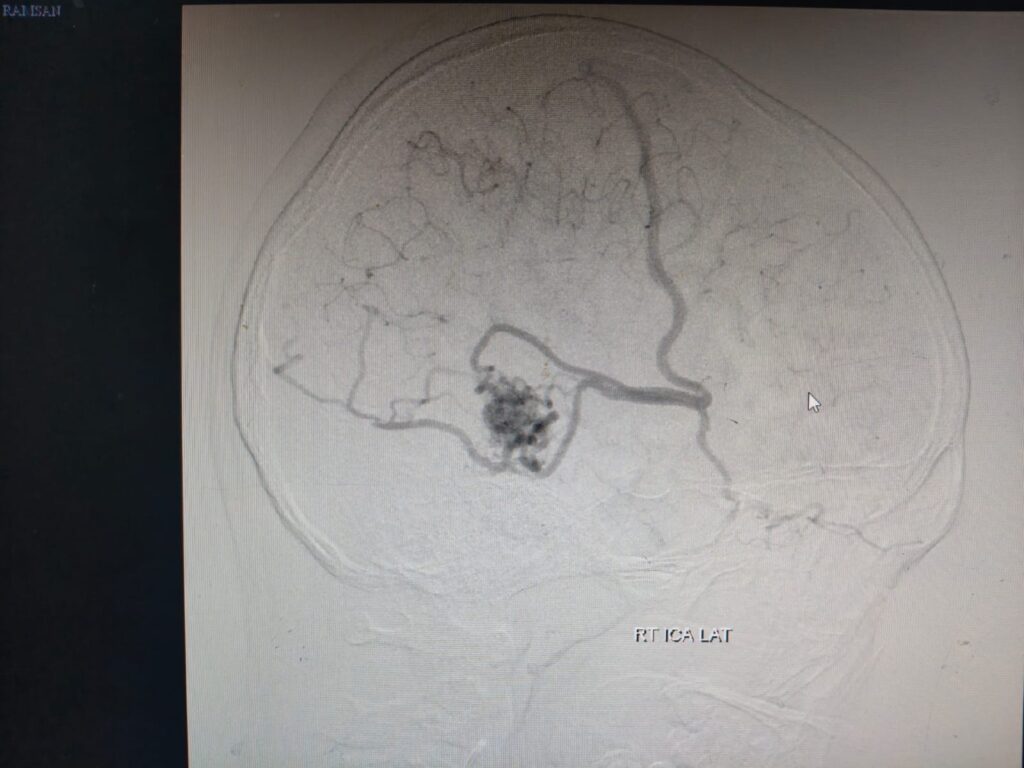
As MRI brain showing Arterio-venous malformation, hence 4 vessel Digital subtraction angiography was planned.
Four vessel digital subtraction angiography :
A compact Arterio-venous malformation in Right Temporal region of size 1.8×1.6×1.6cm with feeders from M4 branches of Right middle cerbral artery with drainage into superior sagittal sinus and Sphenoparietal sinus/Cavernous sinus through cortical veins. No e/o any feeder artery aneurysm/Intranidal aneurysm/venous ectasia. Left Vertebral artery is dominant. No other vascular malformation noted.
Impression: Right Temporal Arterio-venous malformation.
Then child underwent Complete External Beam radiotherapy (CyberKnife -20Gy in single fraction )to AVM .
Currently child is under followup every 6 months – 1 year with imaging to see the progression of disease.
Discussion:
Cerebral vascular malformations refer to a group of conditions characterized abnormal vascular configurations occurring within the brain (and spinal cord). Four general subtypes of congenital malformations include:
●Arteriovenous malformations (AVMs)
●Cavernous malformations (CMs)
●Developmental venous anomalies (DVAs)
●Capillary telangiectasias
AVMs may be subcategorized into pial AVMs and dural arteriovenous fistulas. Cavernous malformations have also been called cavernous angiomas, cavernous hemangiomas, and cavernomas. Developmental venous anomalies were previously also called venous angiomas.
Developmental venous anomalies are most common in autopsy series, with an incidence of 2 percent . This is followed arteriovenous malformations (1 percent), capillary telangiectasias (0.7 percent), and cavernous malformations (0.4 percent). Developmental venous anomalies and capillary telangiectasia are usually benign, while cavernous malformations and arteriovenous malformations have a greater tendency toward neurologic sequelae.
Brain arteriovenous malformations – Arteriovenous malformations are the most dangerous cerebral vascular malformation and can cause hemorrhage, seizures, headaches, and focal neurologic deficits. These lesions are discussed in detail separately.
●Cavernous malformations – Cavernous malformations are thin-walled dilated capillaries with a simple endothelial lining. They may occur as a sporadic or familial condition and may be associated with developmental venous anomalies in about 25 percent.
•Cavernous malformations may be found incidentally on neuroimaging or may present with neurologic symptoms such as hemorrhage, seizures, and/or progressive neurologic deficits .Recurrent hemorrhage is more common after an initial bleed and may be as high as 5 percent per year for supratentorial lesions and 21 percent for brainstem lesions.
•Cavernous malformations are typically identified on MRI and are often angiographically occult. They can occur throughout the brain but are most common in the subcortical rolandic and temporal areas.
•Asymptomatic cavernous malformations are generally followed without intervention. Surgical resection may be indicated for accessible symptomatic lesions associated with progressive neurologic deficits, intractable epilepsy, and/or hemorrhage. Stereotactic radiosurgery is an option for nonoperable lesions, but long-term safety is uncertain.
●Developmental venous anomalies – Developmental venous anomalies (DVAs) consist of a radially arranged configuration of medullary veins separated normal brain parenchyma. The lesions are usually solitary but can be multiple and occur with cavernous malformations.
•DVAs are usually an incidental finding but may rarely present with seizures or hemorrhage. They are usually identified on MRI. Cerebral angiography is considered the gold standard for diagnosis of a DVA. After diagnosis, hemorrhage is unusual.
•Most patients with DVAs are followed without intervention; rarely, surgery is required for hemorrhage or intractable epilepsy.
●Capillary telangiectasias – Capillary telangiectasias are small, dilated capillaries devoid of smooth muscle or elastic fibers. •MRI is the most sensitive imaging modality for the identification of brain capillary telangiectasias . They are most commonly found in the pons, middle cerebellar peduncles, and dentate nuclei. Multiple lesions are common.
•Capillary telangiectasias are usually clinically silent, found incidentally on neuroimaging studies. They are not associated with morbidity, and intervention is not required.
