Dr.Sruthi Suresh, Dr.Sheela Nampoothiri (Paediatricgenetics), Dr.C.Jayakumar
AIMS, Kochi
Three year old male child case of global developmental delay presented with high grade continuous fever and wet cough of three days duration.
He is the 2nd child of 3rd degree consanguinity born out of IUI conception with history of one spontaneous abortion at 8 weeks of gestation.
One sibling death at 7 years of age with similar history of global developmental delay and seizure disorder whose chromosomal microarray was reported as 16p11.2 deletion.
Antenatal period was stormy with history of abruption at 13 weeks and leaking PV at 34 weeks. 1.83kg ba was delivered LSCS due to foetal distress and ba had no asphyxia.
Child was on multidisciplinary follow up for developmental delay from six months of age.
As recalled mother sitting with support one year and walking with support at three years of age. Currently wave’se e at three years of age, follows simple commands and say bisyllables.
Immunised as per IAP schedule.
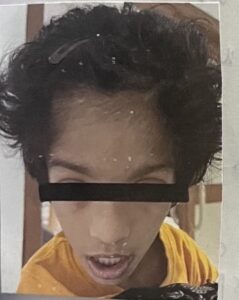
Clinical exam found that he is bed bound with facial dysmorphism.
Vitals and PICCLE were normal.
Head to foot evaluation: Inverted triangular facies, thin upper lip, long philtrum, broad forehead, flat occiput, normal hairline, long fingers and toes, lower limbs- 2nd toe over riding and flexed posture with normal male external genitalia with bilateral descended testes.
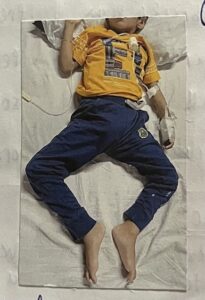

Auxology : His weight was 11.5kg (<3rd centile), length was 105cm (90th-97th centile), head circumference of 50cm.
Neurological examination showed bilateral convergent squint, bilateral loss of bulk, hypotonia of all four limbs, observed power of 3/5 with ellicitable reflexes and equivocal plantar flexor response and involuntary movements.
Examination revealed LRTI.
Blood investigations showed leucocytosis with elevated inflammatory markers (CRP-59.62mg/L).
Chest –X ray showed presence of right paracardiac infiltrates.
His LRTI was managed with piptaz as he was not improving with Amox-clav and supportive and he improved.
VEEG was done which showed left temporal epileptiform abnormalities.
MRI brain reported as generalised neuroparenchymal atrophic changes. As the phenotypic features were consistent with UNC 80 deficiency and WES of parents (3rd degree consanguinity) identified heterozygous carriers for UNC 80 gene along with reanalysis of clinical exome of the child which revealed homozygous for UNC 80 gene.
UNC80 deficiency presents with developmental delay, neonatal hypotonia, severe intellectual disability, dysmorphicfacial features, strabismus, dyskinetic limb movements, and neurobehavioral manifestations. Most affected individuals do not attain independent walking. Seizures may develop during infancy or childhood.
Additional features include clubfeet, joint contractures, scoliosis, postnatal growth deficiency, increased infection risk, sleep disturbances, and constipation. Developmental skills are acquired slowly without signs of neurodegeneration.
The diagnosis of UNC80 deficiency is confirmed in a patient showing characteristic symptoms and having two pathogenic variants in the UNC80 gene identified through genetic testing.
Management involves symptomatic care, including developmental support and education. Melatonin and risperidone can help with sleep issues. Standard treatments are used for irritability, seizures, spasticity and dyskinesia. Feeding therapy or gastrostomy tube feeding may be required. Constipation is managed conventionally. Orthopaedicabnormalities may be treated with braces or corrective surgeries as necessary.
UNC80 deficiency is inherited in an autosomal recessive pattern. If both parents carry one abnormal UNC80 gene each (heterozygous), each sibling of an affected individual has a 25% chance of being affected, a 50% chance of being a carrier without symptoms, and a 25% chance of neither being affected nor a carrier.
Genetic testing can identify carriers among family members and enable prenatal or preimplantation testing for at-risk pregnancies.
Consanguineous marriages can lead to an increased likelihood of inheriting autosomal recessive disorders like UNC80 deficiency, where both parents carry the same disease-causing genetic variant. This highlights the importance of genetic counselling and testing in consanguineous couples to understand and manage the risk of inherited diseases in their offspring.
