Dr.Sree Lekshmy.S, Dr.Sajith Kesavan, Dr.GreeshmaIssac, Dr.C.Jayakumar
One and a half year old female child, first born of a non consanguineous parentage presentedwith recurrent episodes of LRTI since 1yr of age.Child was previously evaluated in multiple hospitals. Chest xray showed persistence of left hemithorax opacity with hyperinflation on right side.
At the time of admission, child was alert with stable vitals. Clinically child had reduced air entry on left.
Differentials considered were:
1.Consolidation
2.Pleural effusion
3.Atelectasis
5.Structural malformations of the left lung
In view of persistence of left hemithoraxopacity,
Flexible Bronchoscopy was done which showed membranous stenosis of left main stem distal end
Using cryo a small hole was created in the membrane but complete recanalization was not achieved since distal lumen was not visible.
Bronchoscopicbiopsy showed fibrocollagenous tissue focally lined squamous epithelium and sub epithelium shows many thin walled vessels and fibroblastic proliferation with few scattered histiocytes, lymphocytes and hemosiderin deposits and no evidence of malignancy.
Later rigid bronchoscopy was done which showed almost complete stenosis of distal left main stem with granulation, with pinhole opening.
Cryoextraction of the granulation tissue followed balloon dilatation with 5G fogartywas done. Post procedure xray showed better aeration of the left lung with persistence of hyperinflation on the right side.
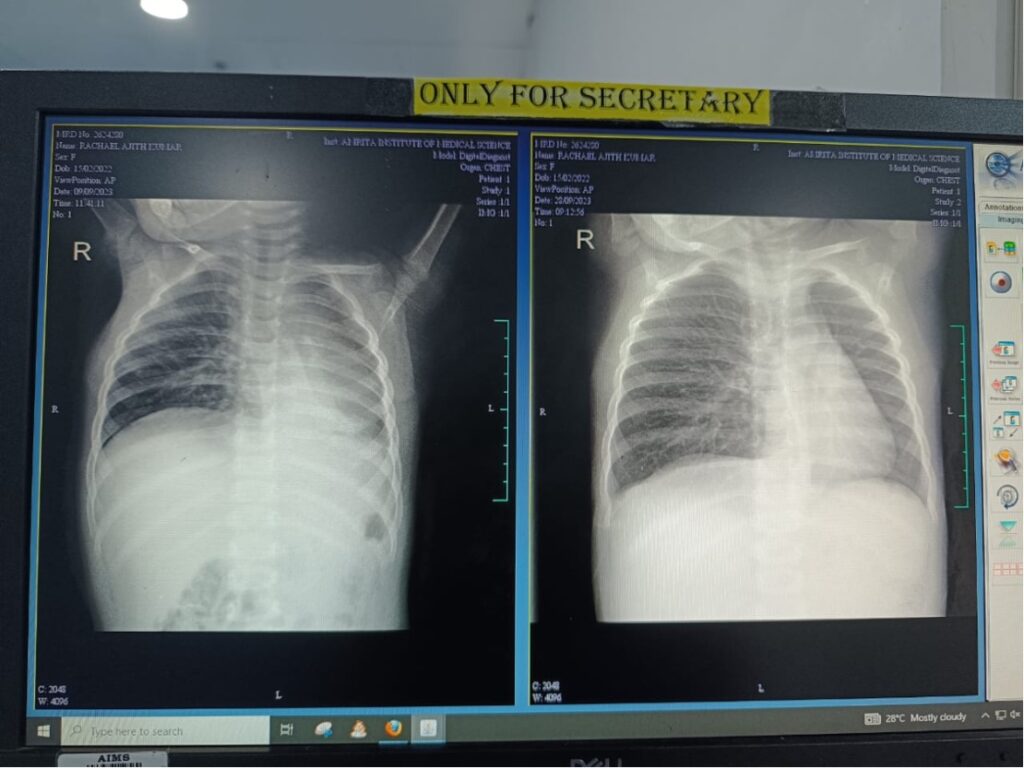
Xray pre and post rigid bronchoscopy
Child was discharged with oral steroids and budesonide nebulisations for two weeks, advised to be on regular follow up and a check bronchoscopy was planned on followup.In this case CT Chest was not done due to the easy access to do Bronchoscopy in the centre
Discussion: A granuloma is a nodular inflammatory lesion comprising of immune cells mainly epithelioid cells and macrophages. They usually form in areas with infection or inflammation. Contact with the tip of an endotracheal tube or suction tube may stimulate the mucosal membrane to form a granuloma. Chronic stimulation or inflammation also encourages granuloma formation, which is often associated with the use of tracheostomy tubes.
A granuloma has been reported in 26% to 80% of tracheostomized patients.
Clinical features include fever, cough with wheeze, sometimes breathing difficulty. Diagnosis is chest xray, CT and diagnostic bronchoscopy. Although there are several treatment options for granulomas, no consensus exists about whether it is preferable to administer steroids intravenously or inhalation, or to carry out surgical excision (with forceps or laser). It has been reported that 60% of granulomas recurred after excision and 48% of unexcised granulomas regressed spontaneously.
Take home message: Early detection, timely intervention and ongoing monitoring are essential to ensure optimal respiratory function. Regular monitoring and imaging are necessary to evaluate the efficacy and assess progression of granuloma.
