Dr.Subbulakshmi P S, Dr.Jayakumar.C, Dr.Vinitha, Dr. Praveena N Bhaskaran, Dr.Suchitra Sivadas.
AIMS, Kochi
Nine year old boy presented with right sided neck swelling for 2 months. It was painless and was gradually increasing in size no h/o fever, weight loss, night sweats, progressive pallor, bleeding tendency ,cough, breathlessness, contact with TB, rash , joint pain
No other swelling noticed elsewhere in the body. Symptoms suggestive of involvement of other system were absent
No h/o medications like allopurinol, atenolol, captopril or phenytoin.
But there is history to of intake of unpasteurized milk present
Also they have a pet-dog at home.
He was Previously healthy with no previous hospital admissions. Developmentally normal, and Immunised up-to date according to NIS. No body in the family had any kind of rheumatological illness or malignancies
Appearance of the child was normal
Vitals normal
No pallor/icterus/clubbing/cyanosis/edema. Right sided multiple discrete posterior cervical lymphnodes –Largest measuring 1.5×1.5cm,non-tender,mobile,firm in consistency.
Oral cavity examination-Normal.
No infection in the drainage area noted
No rashes, joint swellings,no bone tenderness, no significant epitrochlear, axillary or inguinal Lymphnode enlargement. Retina did not show any evidence of chorioretinitis. Systemic examinations were within normal limits.
DIFFERENTIALS:
Viral infection
Allergic disorder
•Infections: Infectious mononucleosis(EBV),
Chancroid,
Toxoplasmosis.
Tuberculous lymph node
• Autoimmune disease:Sjogren
syndrome,SLE,RA
• Drug induced
Sarcoidosis,
Kikuchi lymphadenitis.
Malignancy like lymphoma/Leuakaemia
Investigations: CBC Normal
PS Hypochromic microcytic anemia with mild eosinophilia
Usg Neck:Enlarged cervical lymph nodes on the right(IB,II,V),
FNAC:Reactive LN change,
CXR: No evidence of TB,
Gene Xpert from lymph node for AFB: Negative,
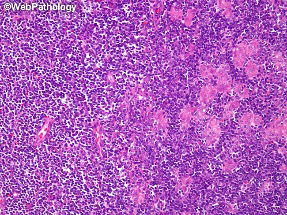
Excisional biopsy: Lymphnode biopsy showing florid reactive hyperplasia with histiocytes collection suggestive of microgranuloma-?Toxoplasmosis.
Serum Toxoplasma IgM:8.45(Reactive), Serum Toxoplasma IgG: >200(Reactive).
This lymph node biopsy image from a case of toxoplasma lymphadenitis shows monocytoid B-cells in a sheet (left half) and aggregates of epithelioid histiocytes (right half).
The child was initially thought to have lipoma in the nape of the neck with lymph node enlargement in posterior auricular region.FNAC was done which showed reactive lymphadenitis after which the child was started on amoxiclav ,the swelling found decreased and amoxiclav was continued. Based on typical histopathology and positive toxoplasma serology, a diagnosis of toxoplasma lymphadenitis was made. Since the patient was an immunocompetent clinically No stigmata of immunodeficiency like deep seated abscess recurrent pneumonia or recurrent Otitis media Fungal infections chronic diarrhoea or any kind of unusual organism isolated from him
Hence decision was made to wait and watch without initiating treatment.
On follow-up Child was maintaining good health and there is resolution of lymph nodes
Treatment
The decision to treat ocular disease is dependent on numerous parameters including acuteness of the lesion, degree of inflammation, visual acuity, and lesion size, location, and persistence. Healed lesions should not be treated. The “classic therapy” for ocular toxoplasmosis consists of the following:
Pyrimethamine 2 mg/kg first day then 1 mg/kg each day, plus sulfadiazine 50 mg/kg two times per day, plus folinic acid (leucovorin) 7.5 mg per day). Therapy should be given for 4 to 6 weeks, followed reevaluation of the patient’s condition. Corticosteroids are sometimes prescribed in addition to antiparasitic agents.
Toxoplasmosis in immunodeficient patients is often fatal if not treated. Treatment is recommended for at least 4 to 6 weeks beyond resolution of all clinical signs and symptoms, but may be required for 6 months or longer. Relapses are known to occur in AIDS patients and maintenance therapy is recommended until a significant immunologic improvement is achieved in response to antiretroviral therapy. Pyrimethamine, folinic acid (leucovorin), and sulfadiazine are standards of therapy for immunodeficient patients.
IMMUNOCOMPROMISED: Serological evidence of acute infection regardless of whether signs and symptoms are present are sufficient to initiate treatment. Therapy should be continued after 4-6 weeks. Beyond the resolution of symptoms. Discontinue maintainence therapy when CD4 >200cells/microlitre.Drugs used are sulphonamides and pyrimethamine.Toxoplasmosis in immunodeficient patients is often fatal if not treated. The dose is ACQUIRED:Pyrimethamine-2mg/kg/day BD X 2days and 1mg/kg/day BD.Sulfadiazine:100mg/kg/day BD.Leucovorin-5-20mg 3 times weekly
Take home message
Toxoplasmosis is an important DD of unexplained lymphadenopathy
Treatment depends up on the site
and extent of
Wait and watch policy is best in case of lymphadenopathy in immuno competent host while treatment is offered inimmuno compromised