Dr. Mahak Bhasin, Dr. Vinitha Prasad, Dr. C. Jayakumar, Department of Pediatrics, AIMS, Kochi
One and half old female , presented with multiple swellings at the back of the head and neck noticed since Day 45 of life with low grade intermittent fever, rhinitis and wet sounding cough of 7 day duration.
There was history of decreased oral intake and decreased urine output of 3 day duration.She was initially admitted at outside hospital and manner with antibiotic and supportive treatment . She developed respiratory distress with low O2 saturation (89% in room air) 1 day prior to admission and hence referred .
Third child of NCM
Mother had overt uncontrolled Diabetes and was on Insulin during pregnancy.
Natal: Term/BW 3.920 kg/LSCS (Polyhydramnious and uncontrolled diabetes)
No history of asphyxia
Postnatal history: History of NNJ on Day 3 of life for which child received phototherapy for 36 hours
She consulted a local doctor and no active management was done.
By 3-4 months of age, the swellings were found to progressively increase in size and beta blockers aided was not given fearing adverse events
2D Echo and ECG done were told to be normal.
At 8 months of age, child developed another swelling on the opposite side of the neck . She was thus shown to a Neurosurgeon and parents advised to wait till 1.6 years old for ?excision surgeries.
History of chest wall prominence noticed the mother in 2 weeks prior to admission.
Family history- Oldest sibling-female, 18 years old- obese, history of a splenic lesion at 16 years of age for which a CECT abdomen was done. Managed medically.
Second sibling–8 years old, male-healthy
No history of early childhood deaths or sudden deaths in the family.
At admission, child was irritable and sick looking. She was afebrile, tachypnoeic and hypoxic.
Vitals: Temp: 97F, PR- 160bpm, RR- 72cpm, BP- 106/72mmHg, SpO2 86% on room air, CRT <2s
Pallor present No icterus, cyanosis, clubbing, lymphadenopathy, edema.
Head to foot examination revealed-
Multiple swellings on nape of neck and occiput of head.
Occiput of head–well circumscribed, 5*5cm non erythematous soft cystic non fluctuant non tender
Nape of neck multiple swellings diffuse on the neck of neck–non tender, non erythematous
BCG Scar was present
No Facial Dysmorphism present
Auxology- normal
Systemic examination revealed bilaterally scattered wheeze and firm liver with normal span that was palpable 4cm below the RCM.
Investigations-
Normal counts with lymphocytic predominance and negative CRP and anemia (8.9g%).
LFT/RFT/SE were normal.
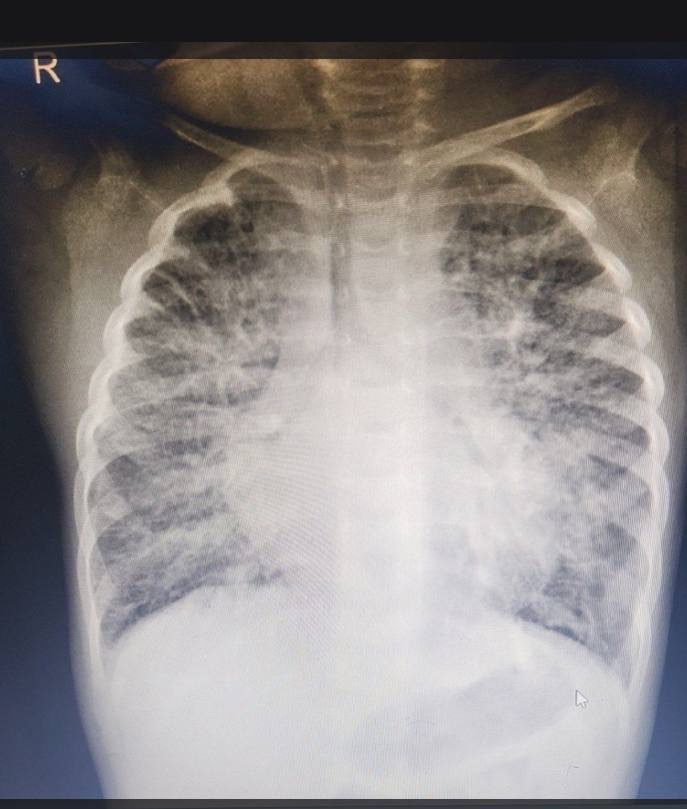
Xray Chest- diffuse heterogeneous bilateral opacities
Xray STNL- straightening of spine with increased retropharyngeal space.
RVP- Negative
Urine Culture- Sterile
Blood Culture- Sterile
USG Abdomen- Normal
As infectious workup was normal, child was thus planned for a CECT head and neck to exclude any internal extension of the lesions of the suboccipital lesions as the cause for the respiratory distress.
She was shifted to the PICU where she was started on HHHFNC with 18L flow and FiO2 of 40%. After sending blood culture, she was started on Inj Ceftriazone and Azithromycin along with nebulised bronchodilators and other supportive measures. She was started on spironolactone and furosemide following which she improved and supports were slowly tapered off to room air. 1 unit of PRBC transfusion was also given as her Hb after admission dropped to 6.7 g%.
CECT head and neck angiogram done showed lobulated low density lesion in suboccipital region with extension along post auricular region and neck shwoing multiple dialted tortous vascular
? venous channels ultimately draining into hugely dilated Left IJV- findings suggesting a venous malformation. Extensive cervical, pre/ paravertebral cluster of dialted tourous vessels along with relative non enhancing ill defined extensive low attenuating lesions in neck , chest wall and mediastinum as described in text.
Overall findings suspicious for a complex mixed venolymphatic malformation.



Mediastinal component encasing mediastinal vessels and airway. No significant luminal compromise.
Patchy lung infiltrates with extensive right lung peribronchovascular / interlobular septal thickening- ? secondary to lymphatic / venous obstruction/ lymphangiectasia.
Pulmonary vein stenosis on right and left inferior vein associated with focal ectasia.
2D Echo done showed normally connected pulmonary veins with significant stenosis at communication with LA.
RA/RV dilated
Small ostium secundum ASD shunting bidirectionally Severe PAH. Systemic septal position. No pleural/pericardial effusion.
Pediatric Cardiology consult was availed. ECHO & CTPA reviewed showed ectatic proximal right sided pulmonary veins with web with diffusely small distal pulmonary veins bilaterally.
A multidisciplinary meeting involving pediatric intensivist, Paediatric cardiologist , pediatric genetics and paediatric surgeon was conducted. It was proposed to do a tissue biopsy for gene mutation studies and start the patient on Sirolimus, After explaining the risks and benefits to the patient. Active cardiology intervention was deferred due to the high risk involved to the patient in any such procedure.
Patients parents requested for discharge as they wanted to go for second opinion at another centre.
Patient was thus discharged at request. She was shifted to another centre where underwent a procedure for Pulmonary Stenosis.
Venolymphatoc Malformations is a descriptive term for vascular malformations comprised of dysplastic venous and lymphatic channels.
50% of these malformations occur at the head and neck region, particularly within the posterior triangle or submandibular regions.
Lymphatic malformations are mostly attributed to the separation failure of embryonic lymphatic systems.
This rare case highlights a constellation of vascular malformations that have not yet been documented in literature. No diagnosis barring the CECT diagnosis is available for the patient and the prognosis remains poor with high morbidity and inevitably early mortality for the child.
