Dr Anakha V Ajay Dr Mahesh K(Dept of Pediatriccardiology) Dr C Jayakumar(Dept of Pediatrics) AIMS, Kochi
Sixteen day old, term male ba born birth weight of 2.8kg with uneventful perinatal history, referred due to tachycardia with HR up to 230/min,. Ba was given Adenosine(3 doses) and was on oralPropranolol @ 5 mg per kg per day.Ba had no history of fast breathing, cyanosis, feeding difficulty.
No family history of heart diseaseor sudden deaths
On examination, ba appeared alert and comfortable. Ba was well perfused with blood pressure of 62/54 mmHg, heart rate of 230/min maintaining saturation at room air and not tachypneic with respiratory rate of 39/min.
CRT less than 2 seconds and peripheral pulses palpable.
Cardiovascular examination revealed normal S1 and S2 split with no mummer appreciated.
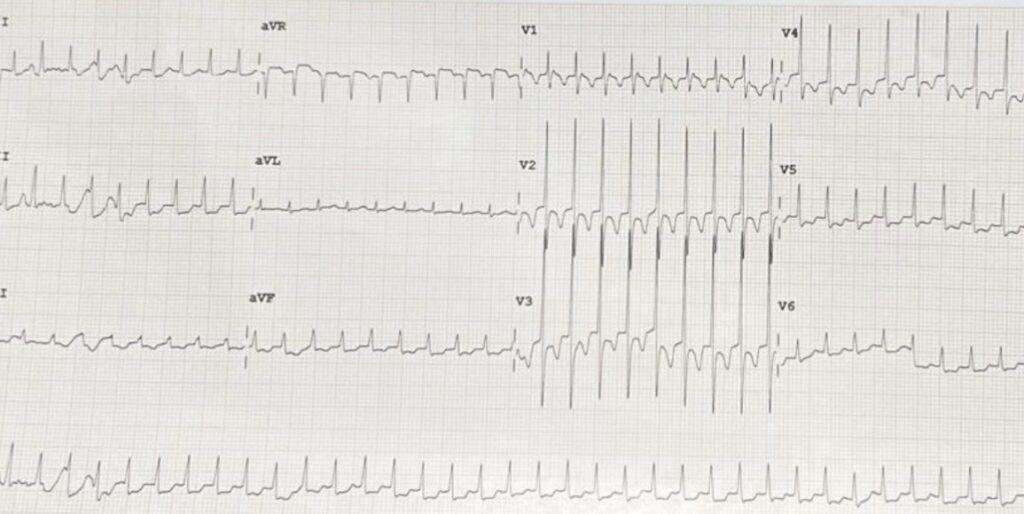
ECG done showed narrow complex tachy arrythmia suggestive of SVT.
Admitted in the IMC and three doses of IVAdenosine(0.1mg/kg) were given but rhythm did not revert. Ba was then started on Iv Metoprolol Infusion, after which reverted to sinus rhythm. Later oral beta blocker (Tab Sotalol) was added and optimized over the next two days with QTcmonitoring.
ECHO done was normal. Baseline investigations were done, which were within normal limits. Patient remained hemodynamically stable throughout the stay and was on direct feeds, at room air.
Regular ECG were done and QTc were within normal limits
Once the patient did not have any runs of tachycardia for 48 hours, ba was discharged on oral beta blocker and advised to be under regular paediatriccardiology follow up.
Emergency management of supraventricular arrhythmia:
Evaluation: Provide oxygen and ventilation immediately as needed and to identify the unstable patient; distinguish SVT from sinus tachycardia.
Clinical assessment:
▪ Potential causes of sinus tachycardia (dehydration, fever, pain, drugs).
▪ Signs of poor perfusion (poor capillary refill, hypotension, pallor, diminished mental status).
▪ Signs of heart failure (increased work of breathing, rales, hepatomegaly).
The following are ECG changes consistent with SVT:
▪ Rate – Infants 220 to 280 bpm; children and adolescents 180 to 240 bpm.
▪ Relentlessly regular rhythm without variation with respiration or activity.
▪ Abnormal P waves (absent or negative in II, III, and aVF).
▪ For wide QRS complex, assume the origin is ventricular (although in children, most are SVT with aberrant conduction)
Children with SVT who are stable are unlikely to deteriorate suddenly, hence begin treatment with vagal maneuvers and/or adenosine and consult pediatric cardiology.
▪ Vagal maneuvers – For infants, apply bag containing ice water to the face above the nose and mouth for 15 to 30 seconds. Do not obstruct ventilation. In older children, bearing down or blowing into an occluded straw for 15 to 20 seconds provides vagal stimulation. Do not use carotid massage or orbital pressure.
▪ Adenosine – With continuous ECG monitoring, administer rapidly through IV closest to the central circulation. Initial dose: 0.1 mg/kg (maximum 6 mg); if no response in 2 minutes, repeat dose 0.2 mg/kg (maximum 12 mg). Follow each dose immediately with a saline flush of 5 mL
For unstable patients (depressed consciousness, poor perfusion, hypotension, or other signs of shock or severe heart failure), begin treatment to convert to sinus rhythm immediately. Continue oxygen and ventilation as needed.
• Adenosine – If immediately available, adenosine may be given to unstable patients with narrow complex SVT with IV access while preparing to cardiovert. Initial dose is 0.1 mg/kg (maximum 6 mg); if no response in 2 minutes, repeat dose 0.2 mg/kg (maximum 12 mg). Follow each dose immediately with a saline flush of 5 ml.
• Synchronized cardioversion – If adenosine is not immediately available or if there is no response to adenosine, synchronized cardioversion should be performed in all unstable patients with IV access. Use 0.5 to 1 J/kg. If not effective, increase to 2 J/kg.
• IV antiarrhythmic options for refractory SVT – Alternative second-line agents that have been used in this setting include IV amiodarone, IV esmolol, IV procainamide, IV sotalol, and IV verapamil (in patients ≥1 year old). Choice of a second-line agent should be guided expert consultation, given potential proarrhythmic and life-threatening hemodynamic collapse when administering multiple antiarrhythmic agents
If IV/IO access is not available, then synchronised cardioversion may be given
Take home message: To recognise SVT promptly and to initiate vagal manures and adenosine treatment urgently and to monitor closely for complications.
