Dr. Terencia/ Dr. Vinayan/Dr.Vaishakh Anand(Dept of Pediatric Neurology)/ Dr. C Jayakumar(Dept of Pediatrics), AIMS, Kochi
One and half year old boy, 1st child of NCM Term/IUGR-1.86kg and mild motor delay presented with complaints of behavioral issues of 2 weeks withpreceding history of fever with cough/cold 5 days prior this
Other domains except the motor was normal priory to the episode . Febrile episode was associated with elevated BP and seizure
1 day after discharge, the mother noticed that the child is extremely lethargic and poor sleeping spells with easy arousability
Word output also reduced and interactions to parents also stopped . Persistent upward gaze (?occulogyric crises) but no hand/perioral dyskinesias was also noticed
No history of cranial nerve involvement. No squint ,ptosis or facial or facial deviation was also described
Child was started on IV antibiotics(Ceftriaxone), acyclovir and other supportives.
MRI Brain with contrast done showed diffuse white matter changes frontal, parietal, temporal, cerebellar and CC hyperintensities sparing relatively occipital cortex.
EEG on day 1- T4,T5 sharps and spikes EEG on day of admission
TMS-GCMS-Negative
CRP raised
Normal CSF study- 6 lymphocytes, protein 44, sugar normal, GRBS-91
CSF Meningo encephalitis Panel ?not known
CSF Neuro myelitis optica Myelin ologodendrocyte glycoprotein (MOG) and Autoimmune encephalitis panel- Negative
Child was treated with IV methyl Perd at 30mg/kg/day, IVIG at 2g/kg over 3 days, Child was started on Biotin, Thiamine, COQ, Pyridoxine (Mitochondrial cocktail)added After starting treatment Child start improving
.
Differentials
1. Mitochondrial cytopathies
2. Leucoencephalopathies
3. Acute disseminated encephalomyelitis, encephalitis
3. Alexander disease
4. Megalencephalic leukoencephalopathy with subcortical cysts (MLC)
5. Other leukodystrophies, such as adrenoleukodystrophy, metachromatic leukodystrophy, and Krabbe disease.
Auto immune encephalitis
Blood routines were within normal limits, with the exception of low Hb. Ambulatory EEG performed which was suggestive of generalized non-specific disturbances of electrical function.
Rapid Meningitis Panel was negative. Serum GFAP was negative.
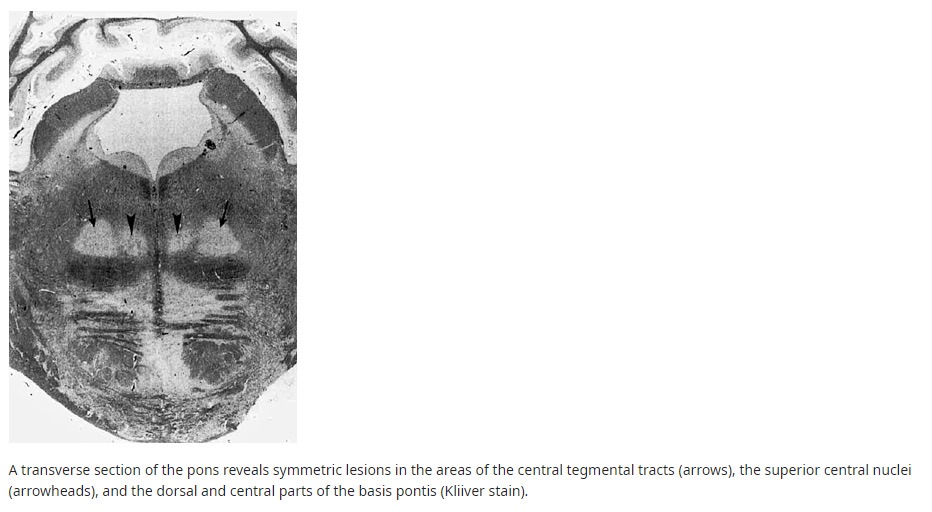
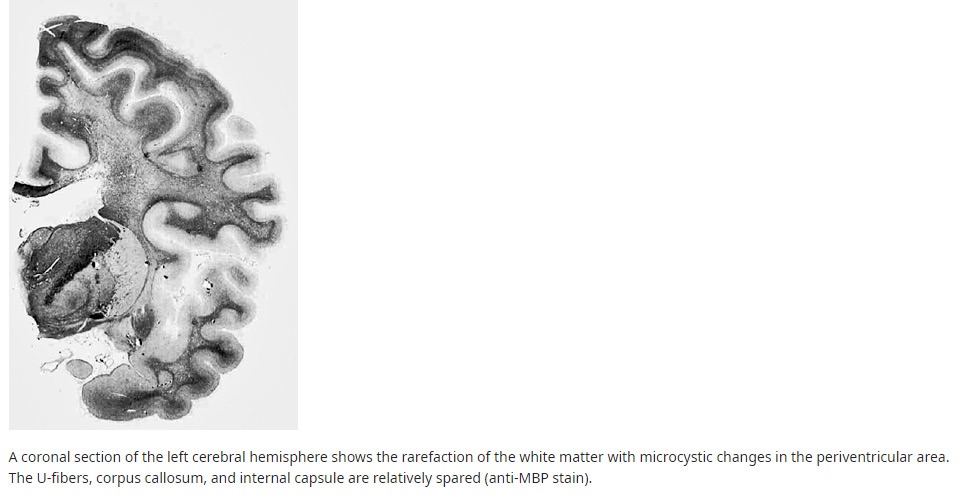
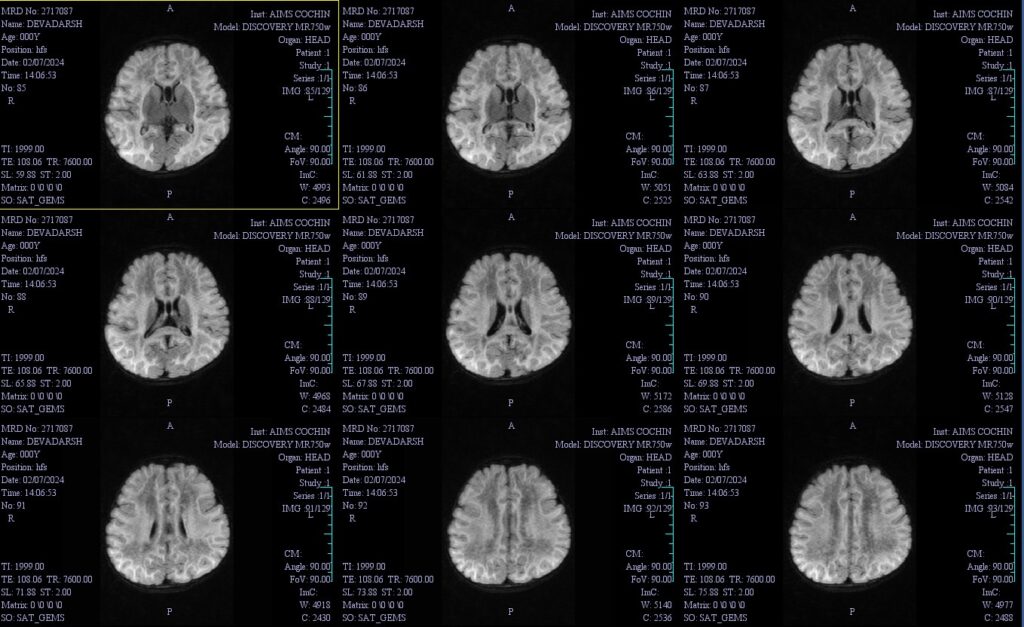
Figure 1-MRI Brain showing-Extensive confluent T2/FLAIR hyperintensity involving supra and infratentorial white matter with few areas of diffusion restriction as described
MRI brain
possibility of a leukodystrophy ?
Vanishingk white matter disease
Mitochondrial cytopathy was also considered
Inj. Methyl Prednisolone was continued and BP was managed with Tab. Clonidine.Levipil was continued along with injectable antibiotics .
Eye ,VEP and NCV were normal.
A gradual improvement was reported
Child was initiated on semi-solid feeds orally after swallowing study . The child is being discharged on NG Tube in situ. His BP values were within normal limits, hence dose of Clonidine was tapered.
Developmental therapy was initiated during the course of the hospital stay. Overall clinical picture was suggestive of Subacute onset encephalopathy following a febrile illness ? Genetic. Possibilities considered were Probable leukoencephalopathies and Mitochondrial Cytopathy. Family is explained in detail about the nature of the child’s condition and the need for the regular follow up.
WES done showed EIF2B4 /homo/Leucoencephalopathy with Vanishing white matter -4/AR/likely pathogenic.
●Definition – Leukodystrophy with vanishing white matter disease is a chronic and progressive white matter disorder with autosomal recessive inheritance, often exacerbated infection or head trauma.
●Genetics – Pathogenic variants in any of the five genes (EIF2B1, EIF2B2, EIF2B3, EIF2B4, and EIF2B5) that encode subunits of the eukaryotic translation initiation factor 2B (eIF2B) are the cause of VWM and its phenotypic variants. These variants usually result in decreased activity of eIF2B, which is thought to disrupt the cellular response to stress.
●Epidemiology – VWM is a rare disease, but it may be one of the more common leukodystrophies. Estimates of incidence range from 1:80,000 to 1:700,000 live-births.
●Clinical features – There are five overlapping clinical subtypes of VWM that exist along a spectrum (antenatal, infantile, early childhood, late childhood/juvenile, and adult). Patients with an earlier age of onset have a more rapid decline. Stressors including illness and minor head trauma often lead to sudden neurologic deterioration with incomplete recovery.
In the early-childhood variant, which is the most common, the major clinical features are progressive neurologic deterioration with prominent ataxia and spasticity. Intellectual functioning and swallowing ability are usually relatively spared. Adults may present with neuropsychiatric symptoms or cognitive decline as their first disease manifestation.
●Neuroimaging features – In early-onset forms, the brain MRI signal of the cerebral white matter changes from high to low intensity on T1 and fluid-attenuated inversion recovery (FLAIR) sequences as the white matter “vanishes” over time and is progressively replaced cerebrospinal fluid (CSF)
These changes are less prominent in late-childhood/juvenile and adult forms. Younger age at onset correlates with increased cystic cerebral white matter decay, while older age at onset correlates with increased cerebral white matter atrophy and gliosis.
Figure 2- Neuropathology of vanishing white matter disease
Figure 3-Neuropathology of the pons in vanishing white matter disease
●Evaluation and diagnosis – The diagnosis of VWM is suspected in patients with suggestive clinical findings and consistent brain MRI findings and/or a family history of disease.
The diagnosis should be confirmed genetic testing demonstrating biallelic pathogenic variants in one of the five causative genes (EIF2B1, EIF2B2, EIF2B3, EIF2B4, and EIF2B5).
●Management – There is no cure or specific treatment for VWM. Supportive care is the mainstay of treatment. Measures to avoid or reduce the risk of events that may trigger deterioration in VWM (eg, head trauma, infection, and fever) are advised.
